This article was originally published on Back to Roots in August, 2021.
A Deep Dive
In May 2021, Dr Craig Liebenson suggested we write a piece for First Principles of Movement (FPM) on how we integrate Play into clinical practice. This put in motion the months that followed where I have chipped away at sharing what we call ‘the Roots’ of helping someone back to play.
This article is written to be saved, reviewed and returned to as a resource for healthcare professionals. We will not be teaching you HOW to play, we will be sharing the theoretical underpinning we have developed, building on the shoulders (see references) of giants before us to help people take play seriously in both rehab and health.
This article will provide you with some of our clinical reasoning, including linked resources to be used by you, and adapted to bring your movement skills out that we don’t even have.
At the end of this article, our hope is that you are empowered to PLAY and empower others to play, the journey really starts then 🙂
Craig, thanks for inviting us to get these points down, keep inspiring.
Luke & the B2R Team

It was estimated in 2010 that persistent pain costs the US economy between 560 and 620 BILLION dollars in medical costs / lost productivity and the care for one person in Australia living with persistent pain between 22588 and 42979 AUD per year.
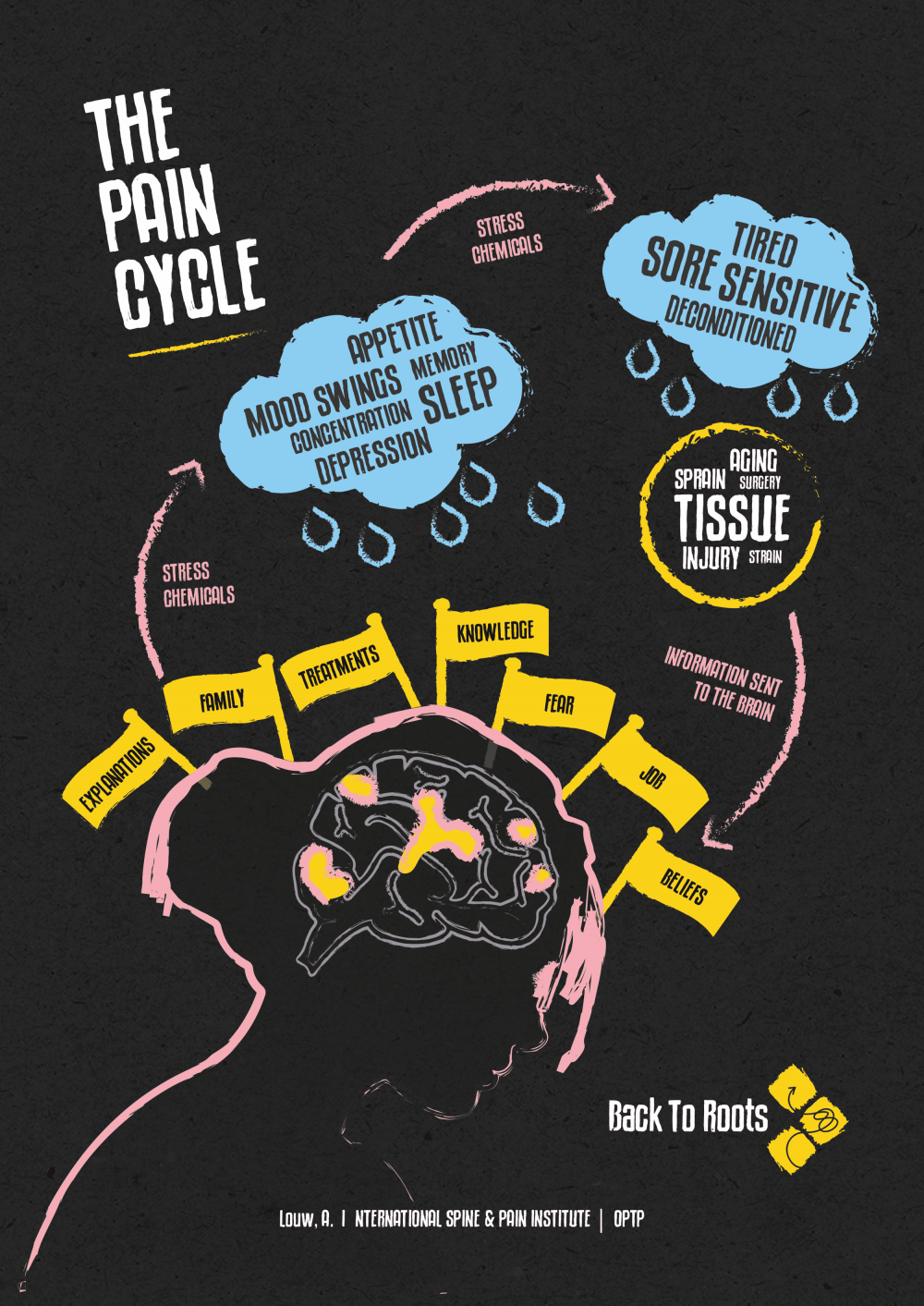
Beyond these soaring economic costs (as reported in the Lancet 2021 series on Chronic Pain) to society the cost to the individual is also significant. Pain is still the main reason people seek medical care (3 of the top 10 including osteoarthritis, headaches and back pain) and chronic pain conditions comprise 3 of the top 4 conditions for years lost to disability (including back pain, neck pain and musculoskeletal disorders). It is also strongly being suggested that persistent pain be treated as a disease in and of itself and in treating this condition there has arguably never been a greater demand for a Bio-Psycho-Social approach.

How do we best do this though? A B2R Perspective
One of the first things we show our students is the Grandfather video that went viral in 2020. This provides a road map of thought processes to guide what is important in rehabilitation. Please take a moment to watch again below.
This short clip really highlights the simplicity of what rehabilitation could be. It all starts with a MEANINGFUL end goal and that is going to come from one place; the person we are helping. Not all clients come with such a clear motivating end goal as shown here and it can be tricky to elicit one beyond being “pain free”.
With a little probing – there is likely something that your client really wants to get back to doing and is actually why they are seeking our help (Ferreira et al., 2010). Spending time and discussing what is truly important to get back to doing is the epitome of shared decision making and is important at all steps along the way (Barry & Edgman-Levitan, 2012). Getting back to this is likely the best outcome measure we have and in doing it together we build therapeutic alliance, self efficacy & resilience (Fu et al., 2018).
Once we are not primarily limited by pain, what activity are you doing again?
— Helpful Goal Setting Question
This end goal serves as our GPS a little like planning a road trip. Seeing the programme birds-eye like this enables the direction we take to emerge as our client progresses; or not. We are aware of the end destination and a rough time that we need to arrive by; however actual decisions along the way may change based on weather, road closure, or even an issue with the vehicle. This is a helpful analogy for keeping us adaptable and nimble in structuring non-linear pedagogy and guides us with overall programme design; in session and between sessions (Renshaw et al., 2019).

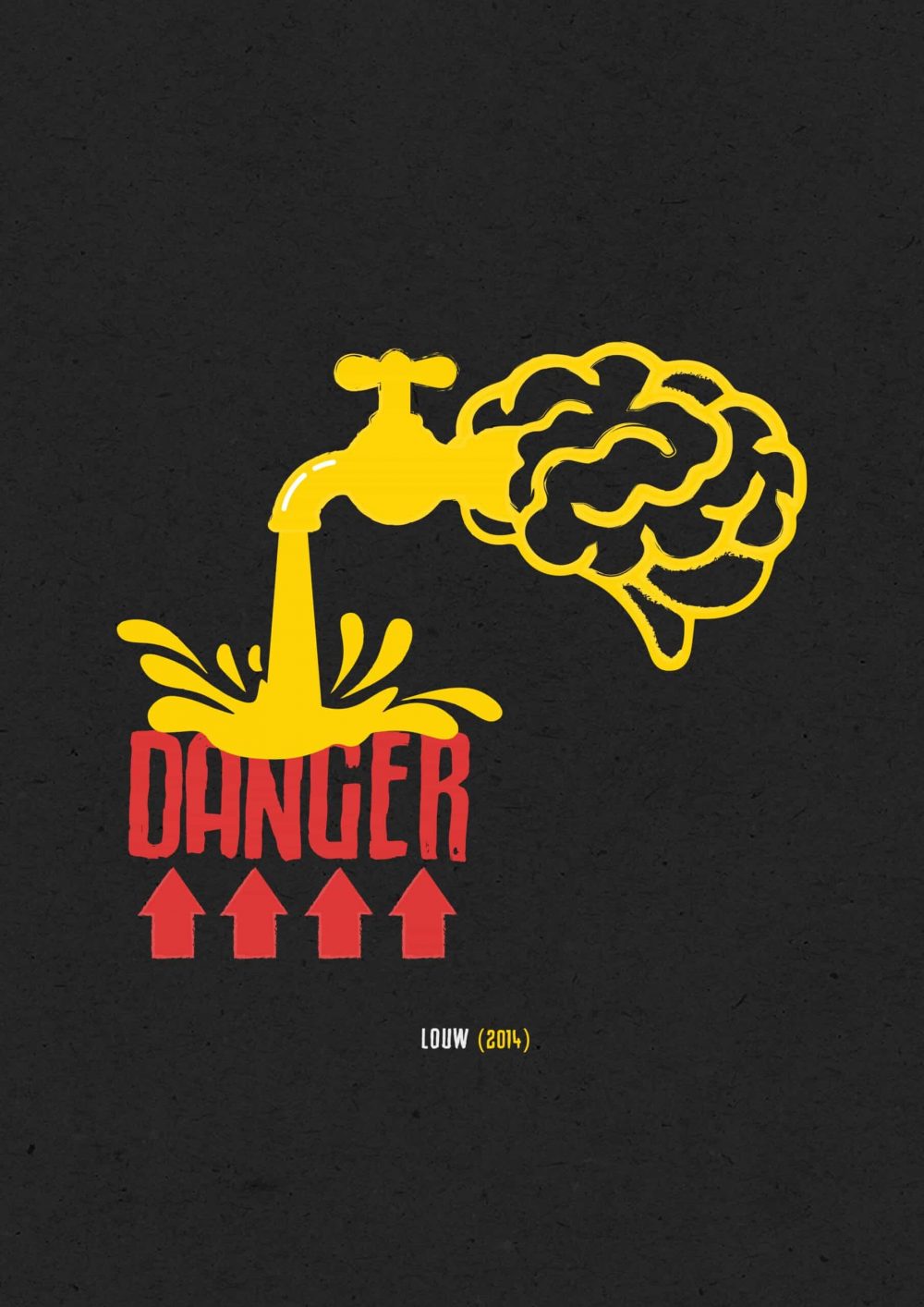
Regarding aches & pains it is worth reviewing that serious pathology (Red Flags) are indeed rare (<1%) in musculoskeletal rehabilitation and should always be ruled out as part of your thorough assessment (Cashin et al 2021). This will also reduce over medicalising pain and the inappropriate medical care that have inevitably followed; MRI / imaging, injections, surgery (Grunau et al. 2017).

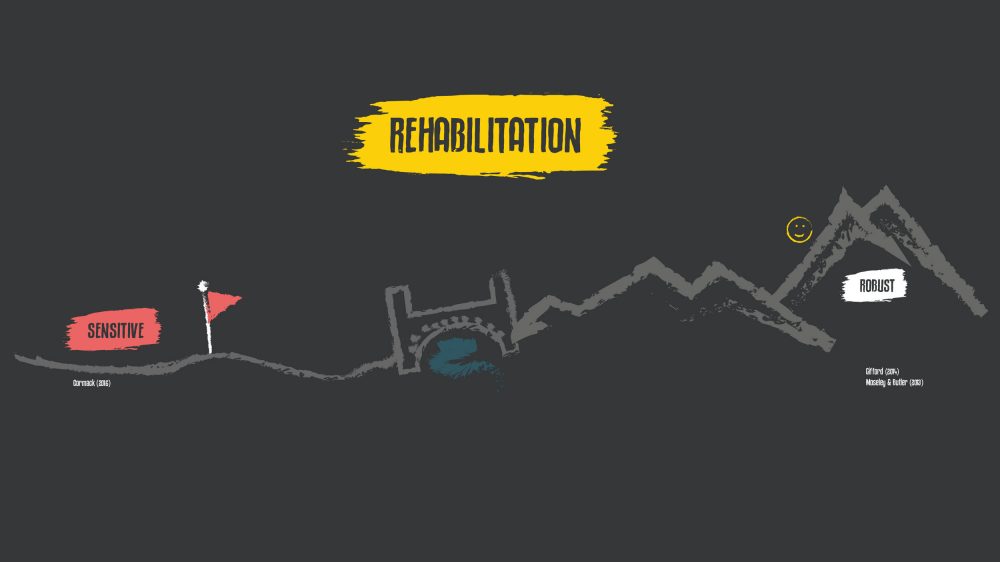
Adaptations at all levels of the nervous system, from the peripheral nerve all the way to the cortex of the brain can be achieved and are perhaps best described by the late great Louis Gifford as “top-down during bottom-up”. We cannot reduce rehabilitation to simply giving exercise (bottom-up) any more than we can talk someone better (top-down) and is the essence of Cognitive Functional Therapy (CFT) by Peter O’Sullivan’s group. A top-down during bottom-up approach is especially important when we appreciate the difficulty we face in overcoming maladaptive beliefs and psychosocial comorbidities our clients come with (See Caneiro et al 2020).
Beliefs and expectations are so important in a contemporary approach to rehabilitation (Carroll et al 2016). ‘Exceeding a client’s expectations of themselves’ has been described by Jeremy Lewis as a primary goal of the clinician (Theory & Practice, 2021) and facilitates experiential learning. It is helpful to establish expectations early in our initial encounter; consider the question below we have at the top of our new client form and the ABCDEFW pneumonic proposed by Louis Gifford.
What exactly do you expect from coming to see and working with me?
— Helpful Expectation Gathering Question
Gathering Beliefs – ABCDEFW (Gifford, 2014)
Attitudes & Beliefs: “What do you think is the cause of your pain?”
Behaviours: “What are you doing to relieve your pain?”
Compensation Issues: “Is your pain placing you in financial difficulties”
Diagnosis & Treatment: “You have been seen and examined for your pain? Are you worried that anything may have been missed?
Emotions: “Is there anything upsetting or worrying you about this pain at the moment?”
Family: “How does your family react to your pain?”
Work: “How is your ability to work affected by your pain?”
WOW, I cannot believe I was able to do that
— Key response in experientially exposing a client to a task
Evidence-based first-line treatments for aches and pains are unfortunately under-utilised globally in favour of the proven more ineffective passive and/or invasive treatments such as rest, imaging, medications, injections and surgery (Foster et al., 2018). Using the ABCDEFW pneumonic helps us gather the information that enables us to individualise education resources to support someone towards active, high-value healthcare utilisation and ultimately self-management (Fu, 2016). Education or understanding, IS an analgesic and has been described as a treatment unto itself (Smart et al., 2012 In Erb & Shmidt, 2021 p279). If we can reconceptualise unhelpful beliefs we shift the needle in terms of the likelihood of a better outcome for our client and our rehabilitation – More HERE.
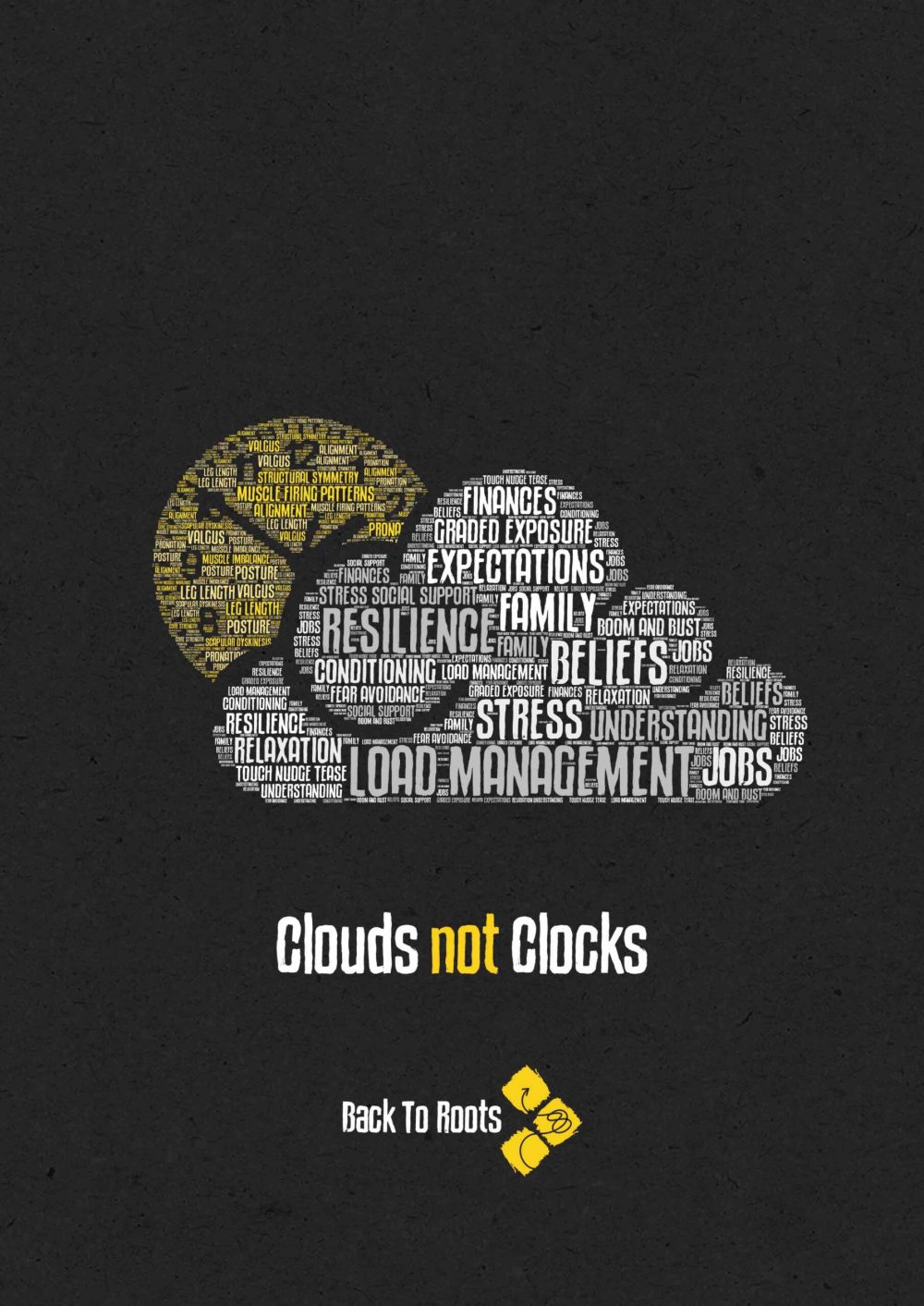
We have created the word art above for helping get across the importance of a bio-psycho-social approach over a biomedical one. Those words that make up the mechanical ‘clock’ are what many will hold as a reason for their pain and unfortunately, significant responsibility for this is due to previous healthcare professionals’ language (Darlow et al., 2018). Those factors in the ‘cloud’ represent some of the important things in a ‘complex’ system we first adapted from Professor Robert Sapolsky (Stanford Lecture Series). If we can support people to be exploring and problem-solving factors in the cloud it is our opinion that we have done a good job in delivering high-value care. Check out the amazing starling murmuration below. This is complex system behaviour in action, just like a cloud, or a human. Luke spoke about this here.
Appreciating these factors is important, we must also be prepared that someone is not ready for their current understanding of their situation to be challenged. We draw on motivational interviewing (MI) literature in this scenario to decide whether to “Comfort the Afflicted – or Afflict the Comfortable”. Some key features of successful MI are shown in the humorous ‘nail’ video below and include:
- Reflective listening skills
- Shared decision making
- Eliciting change talk (we are more likely to act on a decision we made ourselves)
- Validating presentation to show we have heard, without judgement and guide to self discovery
- Resist the desire to offer premature advice or suggestion
Resnicow & McMaster, 2012
It is on the basis that we as healthcare professionals are really in ‘the behaviour change’ game, as Prof Lorimer Moseley describes that the B2R chalkboard was developed, based on motivational interviewing to help shift behaviour through our programmes. We also fully understand the therapeutic value of listening, and spending time which is why the B2R model is not time-limited with our clients, if assessment takes 1 or 3 hours; so be it, if sessions take an hour then that’s what we do (See bottom of article for the chalkboard and bringing it all together).
Some people simply are not ready for their perspective to be shifted, and this is important for us to decide early on as to whether we should even try. The Neuroorthopaedic Institute (NOI) group use the analogy of beliefs being like grains of sand sticking together. Missing bits, single grain, sandcastle, and sandstone as more and more firm beliefs are locked together. Sandstone misconceptions are not yet ready to be challenged, the others however can be done by a nimble clinician. You can read more about these here.
Pain Neuroscience Education (PNE) For Playful Knowledge Translation
Researchers have explored multiple aspects of how PNE can be helpful in the clinical setting. Tailored education about pain helps to shift us away from passive treatments. Level 1 evidence demonstrates that PNE also improves participation in rehab programs, reduces kinesophobia and catastrophizing, and can reduce pain and disability itself. A 2016 systematic review indicated that PNE can improve behaviours associated with pain, fear avoidance, healthcare utilisation and movement. (Erb & Schmid, 2021 p279).
These findings were similar in a 2021 systematic review and meta-analysis concluding that there is more potential benefit in reducing kinesophobia and psychological distress and that these benefits are more likely for the long term than the immediate (Bülow et al 2021). Something worth drawing from the review is the variation in how PNE is delivered. This should give us great confidence in our creativity to be able to bring some of the main concepts to life in our own unique way. To maintain perspective of what these target concepts are delivering we highly recommend reading Cashins ‘Making exercise count..’ (2021) paper linked in the references. We have gathered some of the main target concepts from our ‘curriculum’ below and linked our client resources for delivery.
B2R Implementation Resources
- Pain is a protector & acts like an alarm system – Client Education Implementation
- Tissue damage & pain are not the same – Client Education Implementation
- We can become sensitised, we can also calm nerves down – Client Education Implementation
- Pain is highly multifaceted – Client Education Implementation
- Pain can be influenced substantially by modifiable lifestyle factors – Client Education Implementation
- Movement and pain is variable – Client Education Implementation
- We are bioplastic – Client Education Implementation
- We are a complex system, not a machine – Client Education Implementation
- Tissue Issues may be found in any sensitised body part, but not always relevant –Client Education Implementation for Shoulder, Client Education Implementation for Knee, Client Education Implementation for Heel
This list of target concepts are by no means exhaustive, they are however the basis for our education ‘curricula’ to piece together with a client over the course of a programme (developed in line with that suggested by Moseley & Butler (2019) in their wonderful resource; Explain Pain Supercharged P225. Our curricula can be adapted to be delivered to an individual, or group).
Ecological dynamics provide yet another avenue for exercise and rehabilitation direction; seeing the person and their environment as one entity that despite being perhaps inappropriate logistically, we cannot be ignorant to the idea that behaviour in a clinic is very different from that of real life. When we appreciate the multifactorial nature of pain (remember Moseley’s famous snake bite story), and that neurons that fire together wire together (Hebbian conditioning as described by Gifford, L.) we might appreciate a unique opportunity afforded to Occupational Therapists / OT (who to generalise, work with people IN their context). Do we have to be an OT to apply ecological dynamics in our caseload? Is there a possible opportunity with Telehealth here if we cannot get outside our clinic/gym? B2R example:
The target concepts provided here enable us clinical reasoning for a wide range of exercises and movements to integrate into our individualised programming from taking walking seriously, aerobic exercise, stretching, mindful movements, isolation or body control movements, strength, novel movements, balance, and problem-solving to context-specific exposure. Louis Gifford provided us with the concept of ‘thoughtless, fearless, relaxed movement which perhaps is clinical reasoning in and of itself to work towards as an end goal.
Thoughtless, fearless & relaxed movement is perhaps an end goal unto itself
— Louis Gifford
The EXACT movements or exercises we choose are not that critical and should depend on our patient’s end goal and the repertoire we can actually provide (Oliveira et al., 2018). These are the recommendations of the European Spine Journal and the basis of Callie & Sam (picture way back at the top of article) investing in capoeira to broaden their repertoire and increase their confidence in prescription (Thompson et al., 2020).
I personally have been investing in my skillset for many years now, immerse and move on; rugby, Strength & Conditioning, gymnastics, climbing, hiking, parkour, capoeira, boxing, ballet, and other dance forms, cycling, running, jump rope, strongman…..(you get the idea). These form the basis of what I draw my ‘play-based tasks’ from in clinical practice, and this will evolve as I do. Having access to a “library of tasks” is something you should start building somewhere. This will enable implementation of a constraint-led, nonlinear approach with your clients (Renshaw et al 2019). There is also a growing nudge towards letting our patients choose the exercise modality which has been shown to increase adherence (Yhonatan et al. 2021) as well as simply enjoying the exercise (Angel., 2018).
Key Support Resources – Options are Important
- Explain Pain in Under 5 Minutes (Below)
- Understanding persistent pain
- Neuroplasticity
- Understanding Stress
It is with all of the above, underpinned by behaviour change, motivational interviewing strategies that we developed the B2R chalkboard – to assist us with as little, or as much required for knowledge translation and buy-in.
You Made It
There you have it, the framework, the ROOTS that underpin our approach to integrating play into rehabilitation. What we are sharing is NOT the easiest way to work. It takes effort, energy, and time however it is our belief that this is all worth it when we can bring a smile back to someone who believed they couldn’t, to be able to play again.
From here it is for YOU to bring to life in whatever way works for you.
Keep moving, keep learning, keep playing, keep inspiring others to play.
Luke 🙂
#B2Rhealth
*PS if these images or posters spoke to you, be sure to check out our bundle deal at the store.
References
2. Renshaw et al (2019) Constraint led Approach, Routledge 1st Ed, Milton Park, UK.
8. Gifford, L. (2014). Aches and Pains, TJ International, Padstow, Cornwall, UK.
9. Louw, A. (2014) PNE Cards
10. Lewis, J. (2021) Theory & Practice 19th Ed. [ONLINE]
18. Erb, M. and Schmid, A. A. (2021). Integrative Rehabilitation Practice; The Foundations of Whole-Person Care for Healthcare Professionals, UK, Singing Dragon, an Imprint of Jessica Kingsley Publishers.
19. Moseley, L. and Butler, D. (2019). Explain Pain Supercharged, The Clinician’s Handbook, NOIgroup Publications, South Australia.