Here is a summary of the key 4 Principles that are the foundation of the First Principles of Movement Approach.
A precision approach is always individualized by learning about the patients goals, expectations, concerns, past history, environment, & social context. When the patient feels heard such motivational interviewing established the necessary empathy to guide a compassionate journey towards return to function.
In this way our plan or program is based on the person’s profile rather than us naively assuming all patients with similar pain or pathology require the same prescription. The PATIENT PROFILE emerges when we perform a Needs Analysis of their required capacity (ie demands) & current capacity. The goal of rehab is to bridge the gap from the floor (current capacity shortfall) to their ceiling (required capacity).
By explaining clearly WHY we are doing WHAT we are proposing this builds trust through relatedness. Such trust is the necessary fuel for the patient to persist (eg grit) through the inevitable ups & downs of the process.
1. Pain & Reassurance ➡️ Return to Participation
To manage pain we use a traffic light metaphor where we avoid Red (7-10) & allow yellow (4-6) to provide REASSURANCE that hurt doesn’t necessarily equal harm & that activity is beneficial even if uncomfortable. This promotes a re-conceptualization of safety vs danger messages about ones diagnosis, imaging results, pathology, tissue health, past injuries, muscle imbalances, stability, etc.
The catalyst to accelerate recovery is graded exposures to feared stimuli as one gradually resumes modified activities. This reduces one’s sense of being FRAGILE. The impact of giving tangible hope & an achievable plan thus mitigates OVER-PROTECTION & further negative sequela from excessive rest.
Thus cognitive-behavioral training builds the pain tolerance line & begins to move foreground pain into the background. If you want your body to feel better feel your body move better! It is the 1st step to PREPARE a person to resume activities & SOCIAL PARTICIPATION. “The first treatment is to teach the patient to avoid what harms him”. Nothing is more deleterious than the idea that you are damaged so reassurance about the safety & efficacy of movement is the first step. “The motion is the lotion” concept must be tested sci
entifically using the CAP to disprove the belief that rest is best, the tissue is damaged or that hurt equals harm.
Measurements: VAS, Yellow Flags, ADLs
2. Reactivation & Function
 ‘
‘
By giving tissue sparing or hygiene advice REACTIVATION is accelerated. In this way we increase contextually relevant exposure & variability while concurrently improving competency & thus self-efficacy! This bridges the gap from preparation to training & from fragility to resilence.
As one regains confidence positive adaptations begin to replace negative compensations of excessive guarding & OVER-PROTECTION. By priming resumption of near normal activities descending fear avoidance beliefs & behaviors are mitigated upstream thus preventing the descent into disability.
Measurements: integrity of movement prep screens or motor control (0-3)
3. Load & Resilence ➡️ Safe Return to Higher Demands.
The next progression is to gradually add load. This is measured with the rating of perceived exertion (RPE) scale. This is an essential hack for RESILENCE by avoiding the tendency to manage patients away from load & fostering rehab purgatory due to UNDER-PREPARATION & inevitable re-injury. By slow-cooking the load exposure RETURN to PLAY & SPORT can safely occur.
Measurements: RPE, RM, capacity
4. Variability ➡️ Return to Optimal Performance
The final progression is to further enrich the contextual exposures by imagining the most unpredictable aspects of one’s life or activities & preparing for the unexpected (Gabbett). This ANTI-FRAGILE message uses the full gamet of Dynamic Systems Theory (DST), attractor states, advanced periodization (shock blocks), accessory exercises, & variability of training optionality (tri planer, different stances, grips, etc).
In this final stage the movement literacies of agility, balance & coordination (ABCs) are trained for long term athletic participation & sustainability in the TASKS & SOCIAL ENVIRONMENT deemed of value by the patient. In this way we seek both to identify upstream solutions & provide behavioral nudges & guardrails gamified for making the hard easy.
Finally, it is always the goal to be as precise as possible. We want to find the source of the source (Pain generator) by seeing the INDIVIDUAL as having a linkage system. Assessment of the regional interdependence of the entire kinetic chain will identify key, relatable “weak links” to be addressed. Since you are only as strong as you’re weakest link this level of mastery is required to OPTIMIZE PERFORMANCE sustainably & thus reduce injury risk. “That which enhances performance prevents injury.”
Measurements: above outcomes for progress
Summary
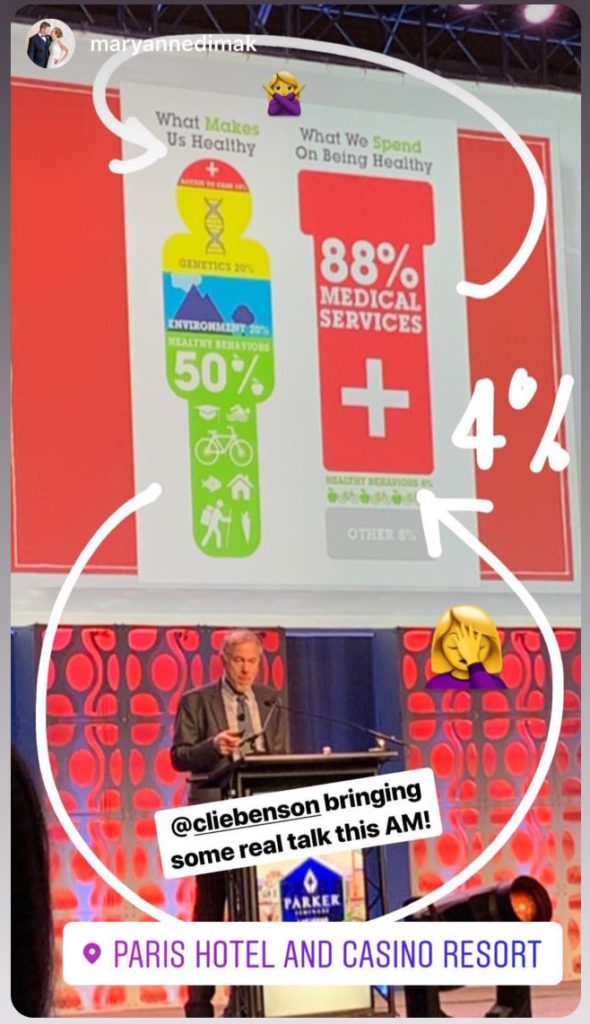
This comprehensive strategy takes a mutivariate approach to enhancing the INDIVIDUAL’S relationship to their ENVIRONMENT & TASKS. By seeing how a linear approach of treating the site of symptoms with palliative measures, or focusing mainly on the pathology (“the tissue is the issue”), is inconsistent with the BPS precision, patient-centered approach we can provide more functional & relatable guidance to patients.
The culmination of the pivot from more rigid Doctor-centered rehab Rx is the shift to more agile patient-centered functional rehab. This compassionate approach recognizes the patients ENVIRONMENT, behaviors & goals, not just their pathology or symptoms.