In a dialogue with Pr Karin Silbernagel I ask “What is the acceptable NRS range for training patients with musculoskeletal pain?”
Background
The Smith, Littlewood paper contends:
“Protocols using painful exercises offer a small but significant benefit over pain-free exercises in the short term, with moderate quality of evidence. In the medium and long term there is no clear superiority of one treatment over another. Pain during therapeutic exercise for chronic musculoskeletal pain need not be a barrier to successful outcomes”
“Traditionally, healthcare practitioners have been reluctant to encourage patients to continue with exercise into pain when they are treating chronic musculoskeletal pain, with some research suggesting clinicians’ fear being the primary deterrent. The results of our systematic review show that there does not appear to be a scientific basis for this fear in relation to outcome measures of pain, and also potentially function and disability. This is an important point when considering what advice is given on any short-term exacerbations of musculoskeletal pain during physical activity or exercise by healthcare practitioners”
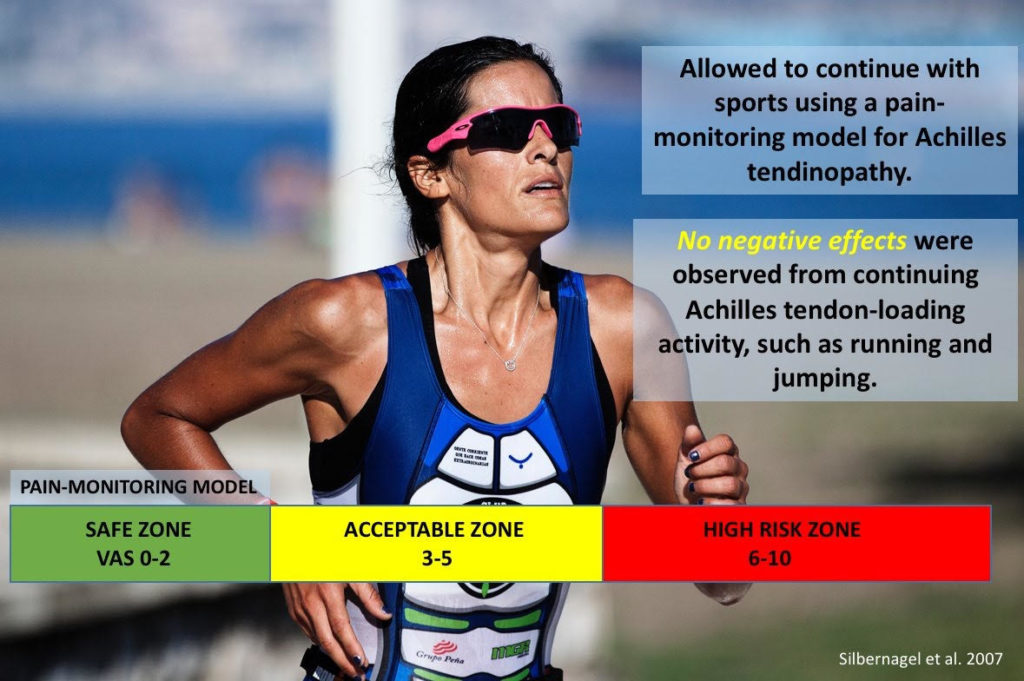
Silbernagel’s paper suggests 3-5 is acceptable:
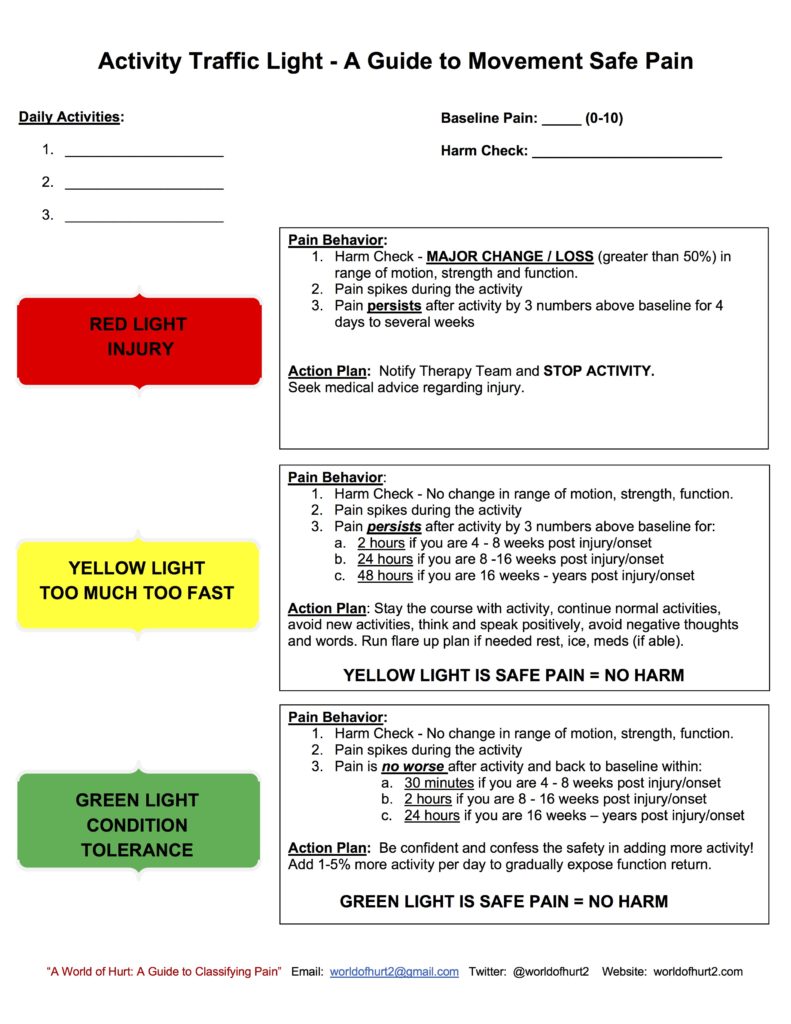
Annie O’Conner has published in her book World of Hurt that a goal is to violate the patients expectancy that hurt equals harm. Especially with yellow light pain.
This is from Annie’ group at the Shirley Ryan Ability Lab:
Kristian Thorberg PhD, PT presenting on groin injuries suggested “yellow light” is ok.
Kristian Thorberg. presentation on groin pain management in team sports. Swiss Sports Physio and Med Conf., Bern, 2018.
Red light – Stop – 6-10 they look like patients. Now you have to actually stop.
Yellow light – Pay attention just like when you are driving. You can chose to cross, but you might get a ticket. Or crash into somebody.
Green light – Go.
However in this groin study Thorberg found “Players were asked to start at level 3 (exercise difficulty for novice). However, if they experienced groin pain during the exercise >3 on an 11-point numeric rating scale…they were instructed to perform level 2 instead.”
& with PFP in adolescents Thorberg suggests < 3 pain intensity was shown to have best outcomes.

In a discussion on Twitter (5/16/19) Thorberg had this to say:
“Yes, for PFP kids we wanted something simpler. OK, not OK. Colour coding and numbers can be discussed, but this tool was to help them stay active without continuing to provoke symptoms, which we identified as a main issue in these patients as pain is associated with poorer prognosis”
Chris Littlewood PhD, PT replied, “Thanks for highlighting research and discussion. Perhaps one concern we do all share is inferring too much from non-randomised studies?”
Pr Karin Silbernagel’s Comments Re: Pain Intensity & Rehab
Karin Grävare Silbernagel PT, ATC, PhD
Associate Professor
Department of Physical Therapy
University of Delaware
STAR Health Sciences Complex Campus
“The original pain monitoring came from Roland Thomee my PhD advisor who did his thesis on Patellofemoral Pain in adults. I then adopted to tendinopathy. The point in my opinion is that we need to help patients understand that the pain in certain conditions are not dangerous. Such as in tendinopathy loading the tendon is painful but the load is needed for stimulating the tendon to recovery so we are less worried about the pain so 5 seems to be the difference between I feel it and Ouch it really hurts (I hope that make sense). If someone has insertional tendinopathy then I might be more restrictive because the pain might be due to compression of for example the bursa and then I might say lower pain is acceptable especially at the position of DF (for Achilles insertional tendinopathy). So when we come to PFP I would also be somewhat more restrictive since we are not sure of what is pain provoking and if the pain is related to Patella positioning. So as I teach all PT students it depends. I often get complaints that 5 might be too much and I say “I really do not care what number you use” as long as you have a reason.
I hope this make sense. To me Biological plausibility/explanation and reasoning ranks high and then you can individualize. Meaning waiting for the pain to subside does not work because you get weaker and the tissue decreases its tolerance to load. So loading with pain is beneficial to get the structures to improve. However if it is a fracture it might be very different so know the injury and tissue.
Same with isometrics, the tendon needs load and probably has no clue what the muscle does (i.e how it contracts) it only knows load magnitude and duration. So you can manipulate best you can and pick the type of loading (contraction) that works for your patient.
My goal is to avoid too many recipes and instead think about the concepts in that way you can handle any patient be it elite athlete or recreational athlete or geriatric.”
What about “if it hurts don’t do it”?
Many people believe the medical adage – “if it hurts don’t do it”. We know that for some this promotes illness behavior by giving the idea that the body is fragile. Ben Smith & Chris Littlewood’s shoulder paper, Annie O’Conner’s WOH book, some of K Thorberg’s groin work, & you’re tendonopathy paper all show yellow pain is acceptable. Ben & Chris seem to have gone the furthest in showing that Annie’s point about “violating one’s pain expectations” is crucial perhaps by altering beliefs about the relationship of “hurt and harm” or “activity & injury or danger”.
I love this comment from Pr. Silbernagel
“Please feel free to disagree or have further questions and email me back. I love scientific discussions and sharing”
Others like Mike Boyle who commented on Chris Littleton’s Twitter post believes “if it hurts don’t do it’. Clearly, he is aiming at knucklehead athletes who believe “no pain no gain”, but the P O’Sullivan, L Moseley advice is quite different for chronic pain sufferers who are iatrogenically sent down the disability road by overly careful activity restrictions & pain avoidance recommendations of well meaning clinicians.
Strength Coach Classic- “Does It Hurt?”
Article from Mike Boyle: Strength Coach Classic- “Does It Hurt?”
“If you have an injury and are wondering whether or not a certain exercise is appropriate, ask yourself a simple question. “Does it hurt”?
The key here is that the question “Does it hurt?” can only be answered yes or no.
If you answer yes, then you are not ready for that exercise, no matter how much you like it. Simple, right? Not really. I tell everyone I speak with about rehab that any equivocation is a yes. Things like “after I warm-up it goes away” etc. are all yes answers……
If you are injured and want to get better, use your common sense. Exercise should not cause pain.
This seems simple but exercisers ignore pain all the time and rationalize it. Discomfort is common at the end of a set in a strength exercise or at the end of an intense cardiovascular workout. Additional discomfort, delayed onset muscle soreness, often occurs the two days following an intense session. This is normal. This discomfort should only last two days and should be limited to the muscles not the joints or tendons. Pain at the onset of an exercise is neither normal nor healthy and is indicative of a problem.
Progression in any strength exercise should be based on a full, pain-free range of motion that produces muscle soreness without joint soreness”
To P O’Sullivan or L Moseley let alone Tim Gabbett this advice would likely be disputed. Mike Boyle’s point may apply in certain cases, but the scientific evidence that it is a principle is lacking. As a student of chronic pain we have clear Yellow Flags such as:
- the belief that hurt equals harm
- the belief that activity is harmful
- the belief that if an activity hurts it should be stopped
The evidence suggest where you draw the line between yellow & red is actually grey. In this grey area K Thorberg’s line rings true to me. “Be cautious – look both ways before crossing.” So we cross. We don’t stop. Now, K Thorberg says in youth with knee issues it’s different than elite soccer players with groin issues. It makes sense to be more cautious with youth. Especially now that he has evidence. But, I wonder if we look at beliefs and attitudes through the yellow flags lens what we might see. Those with overly protective (to use Moseley’s term) thoughts, emotions or beliefs (i.e Yellow flags) perhaps we should reassure them more, thus “violating their expectation”? Further, perhaps if they don’t have these yellow flags pre-existing beliefs we should be mindful NOT to imbue them with these?
The ultimate questions is do we have rules for how to apply common sense so as to nuance the NRS/VAS in different contexts?
OA
OA is an area where work on the NRS & exercise has taken root.
A few points they make –
- The patient decides what’s tolerable.
- Above 5 is red light
- If pain increases with exercise that’s OK so long as by the next day it has calmed.
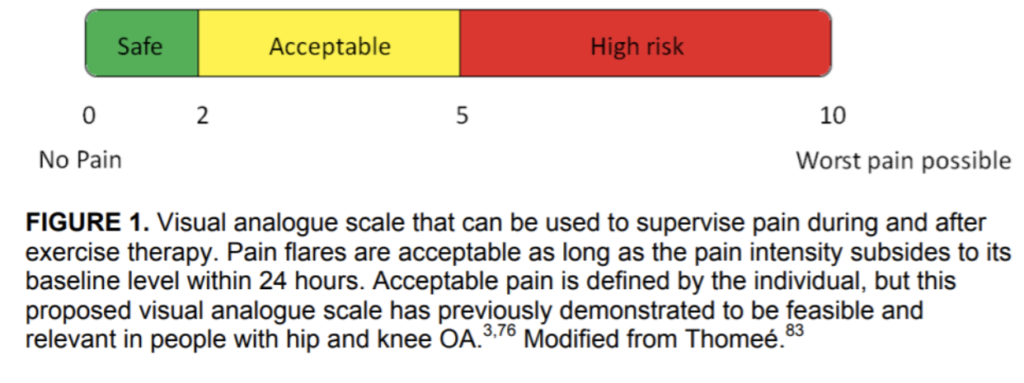
From Silbernagel:
“In reference to pain I think you have to always consider what you are talking about. Such as if I am wearing shoes that gives me a blister I would say don’t continue with pain above 1/10 because the blister will get worse and maybe start bleeding. So same with some exercises feasibly if healthy. However tendon needs load to recover despite load being painful. For knee OA you have pain but loading the knee is not really making the OA any worse (probably) so in order to improve strength and function allow pain to move forward. The main thing as well with the pain monitoring model is that pain should not increase from week to week.
As far as chronic pain you need to also evaluate if (there is) possible central sensitization and then your approach needs to address that.”
Are Pain Tolerance and Pan Intensity the Same Thing?
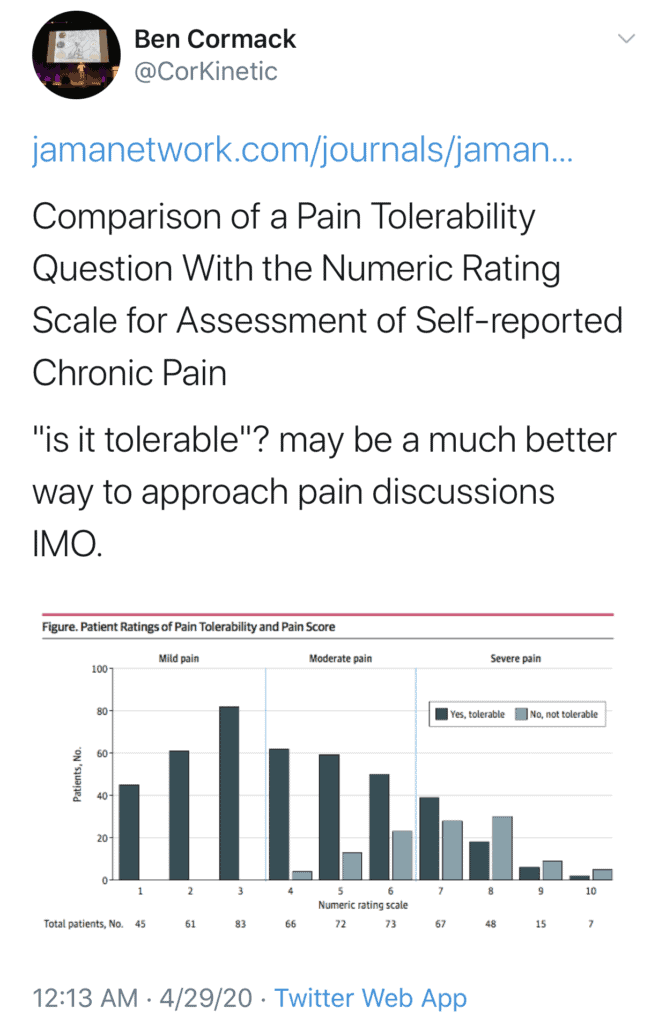
It is crucial to always ask ‘Is the pain tolerable”? Often a patient will say the pain is 9/10. Then when you ask is it tolerable they say “Oh yes”. As you can see in this diagram there are a nuances to asking about pain.
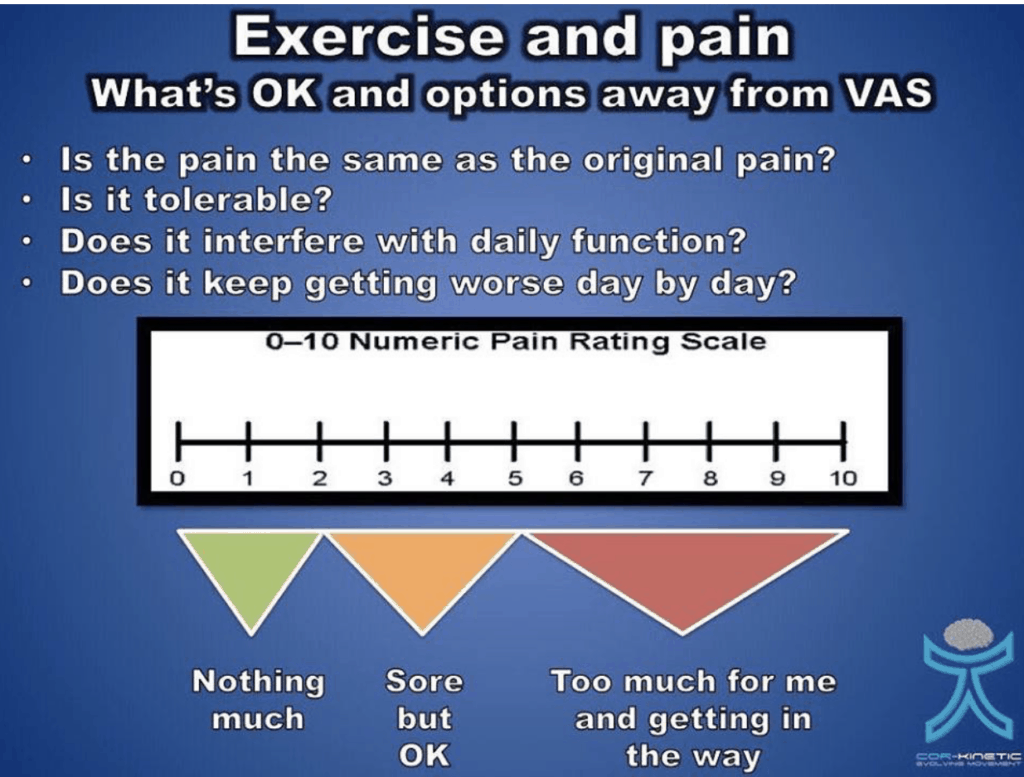
In a new study asking about pain tolerance vs using a Numeric Rating Scale is compared. Ben Cormack suggests the pain tolerance question may be a better way to discuss the complexity of the pain experience.
In the study a number of germane issues are raised.
- “The exclusive focus of the numeric rating scale (NRS) on pain intensity reduces the experience of chronic pain to a single dimension.”
- “This drawback minimizes the complex effects of chronic pain on patients’ lives and the trade-offs that are often involved in analgesic decision-making.”
- “Furthermore, continually asking patients to rate their pain on a scale that is anchored by a pain-free state (ie, 0) implies that being pain free is a readily attainable treatment goal, which may contribute to unrealistic expectations for complete relief.”
The authors go on to explain the benefits of asking about pain tolerance.
- “We hypothesized that the incorporation of a standardized pain tolerability question (PTQ) (ie, “is your pain tolerable?”) would efficiently augment the information gleaned from the NRS and help to align patients’ expectations with realistic treatment goals.”
The modern approach to managing disabling musculoskeletal pain is to shift the focus from chasing symptomatic relief to to addressing activity intolerances related to symptoms.
- “ The overarching goal of chronic pain treatment is to make pain tolerable for the patient rather than to attain a targeted numeric rating.”
- “Our findings confirmed the intuitive assumption that most patients with low pain intensity (ie, NRS score, 1-3) find their pain tolerable.”
- “In contrast, the tolerability of pain rated between 4 and 6 varies substantially among patients.
- “In this middle range, if a patient describes pain as tolerable, this might decrease the clinician’s inclination to initiate higher-risk treatments.”
- “A substantial subgroup of patients with severe pain reported their symptoms as tolerable.”
This discussion highlights that hurt does not necessarily equal harm. Nearly all musculoskeletal pain guidelines over the last 30 years have emphasized that pain does not equal tissue damage or impending injury. This study goes a long way to show us better ways to educate people in reassuring ways that will get them back to activity and thus build a mindset that can make them feel less fragile.
- “Discordance between tolerability and pain intensity may be an opening for a clinician to explore mood, sleep disruption, or the curtailing of activities to control pain.
- “Asking patients with chronic pain about pain tolerability directly addresses the main limitation of the NRS, which asks patients to rate a complex, highly subjective experience on a unidimensional intensity scale.”
Read the study on JAMA Network.
See these 3 articles for some relevant discussion:
Roland Thomeé – Comprehensive Treatment Approach for Patellofemoral Pain Syndrome in Young Women
Jo Nijs et al – Recognition and Treatment of Central Sensitization in Chronic Pain Patients: Not Limited to Specialized Care
Jo Nijs et al – Exercise therapy for chronic musculoskeletal pain: Innovation by altering pain memories



