This opened up new avenues for my coaching. First as a designer of environments and guardrails which challenged the faulty pattern. Second, helping people discover the edge of their capability so they were neither in their “comfort zone” or doing something beyond their current potential. This led me to Dynamic Systems Theory (DST) which states that the individual, environment and task are the three main variables to influence that facilitates transferable skill acquisition.
“When it comes to applying constraints it is helpful to remember that we are trying to discourage one movement so a new movement can emerge. This way the athlete finds the preferred pattern on their own opposed to us telling or showing them.” Nick Winkelman
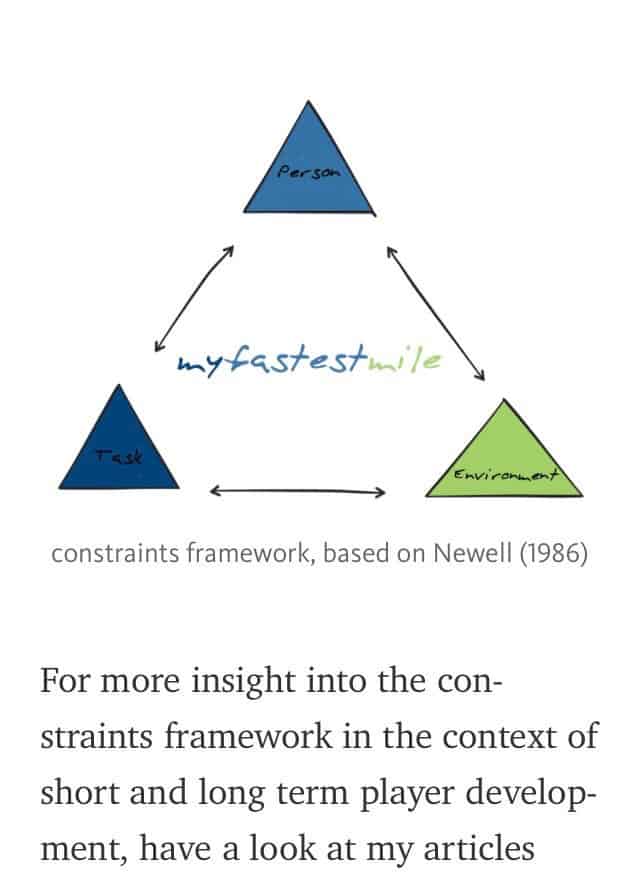
DST has opened me up to the value of uncertainty. There is not just 1 way to do things.

Inter-relationships are broad.
When we utilize the Goldilock’s Principle and avoid either doing things too easy or too hard it helps people gain access to the flow state.

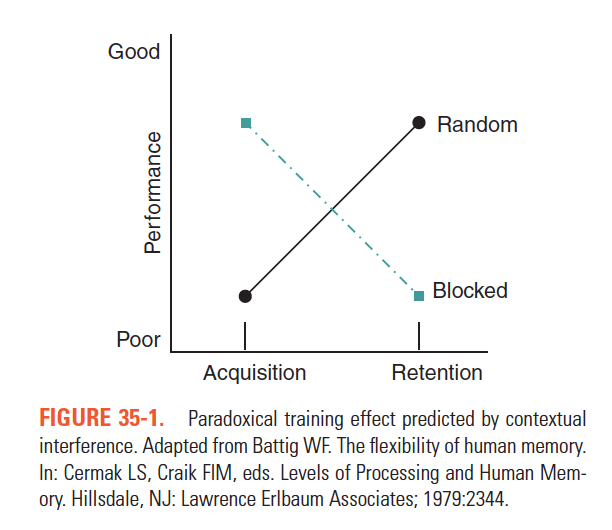
A great deal of literature also exists on how we cue. Gab Wulf’s career has been focused on the difference between internal vs external cues in performance. Prior work on blocked vs random practice also addressed this showing that random practice led to delayed skill acquisition but greater long-term retention than blocked. External cues are often visual images or metaphors and these have proven repeatedly to be superior to internal cues (see below Rich Willy, PT, PhD’s work).



A fascinating example of motor learning in anterior knee pain:
Mirror gait retraining for the treatment of patellofemoral pain in female runners
Willy RW, Scholz JP, Davis IS. Clinical Biomechanics. 27, 2012. 1045-1051
see article (Willy RW mirror retraining 2012.pdf):
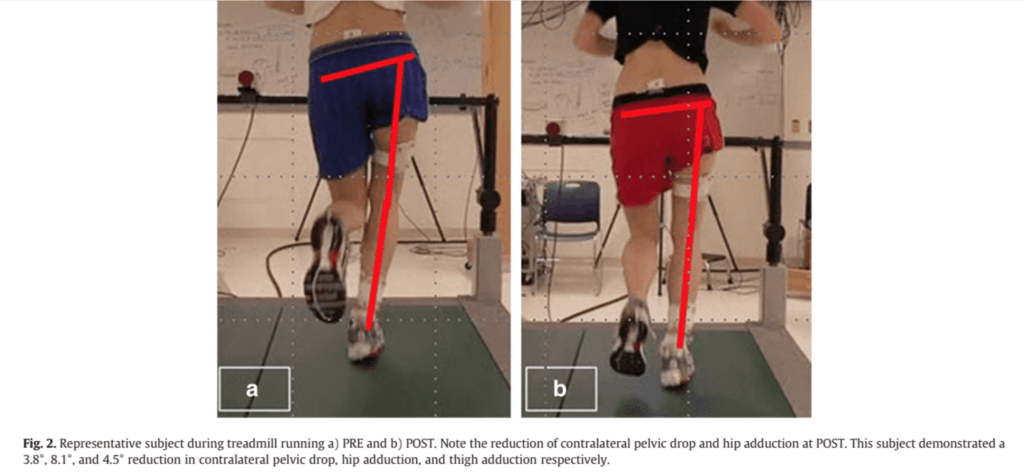
Gait retraining in female runners with PFP, using a full-length mirror, resulted in significant improvements in pain, function, and abnormal mechanics from their baseline measures. The new movement skill transferred to the untrained tasks of single leg squat and step descent, thus indicating acquisition of a new motor skill. Reductions in pain, function, and mechanics were generally maintained through 3 months, suggesting potential for long term changes. The results of this study are promising, as this technique requires only a treadmill and a full-length mirror.
Those subjects who demonstrated abnormal hip alignment during running were invited to participate in the gait retraining phase. Abnormal hip alignment during running was operationally defined as peak HADD greater than 1 standard deviation above the mean of our lab’s normative database of running (peak HADD qualifying criterion=20°).For qualified subjects, data collected during the kinematic screening served as their baseline data for the gait retraining protocol. Runners who did not meet this kinematic inclusion criterion were dismissed from further participation in the study.
Participants who met the kinematic qualification criteria attended a total of eight gait retraining sessions over the course of 2 weeks.During the first training session, subjects were first shown their baseline video so they could visualize the abnormal hip and knee alignment that they exhibited during running. During gait retraining, visual feedback was provided by a full length mirror that was placed directly in front of the treadmill. Participants received scripted verbal cueing at the beginning of each session, consisting of “run with your knees apart with your kneecaps pointing straight ahead” and “squeeze your buttocks.
Feedback exposure and treadmill runtime were tightly controlled. Runners attended 8 retraining visits over the course of the 2 weeks, during which treadmill runtime was gradually increased from 15 min to 30 min (Fig. 1). This schedule is based on previous studies (Barrios et al., 2010; Crowell and Davis, 2011; Noehren 2011). Feedback was gradually removed during the final 4 training sessions, in accordance with the feedback schedule, to shift dependence from external to internal cues and reinforce learning (Winstein and Schmidt, 1990). This was accomplished by decremental reductions in verbal cueing in addition to reductions in visual feedback by turning the mirror around so that subjects could not see themselves while running.
During each period of feedback removal, running mechanics were monitored via a standard video stream that was only visible to the investigator. Once feedback was resumed, runners received retrospective verbal cueing on their running mechanics during the preceding feedback removal period. To ensure that feedback was consistent across subjects, runners were not permitted to run outside of the lab while participating in the gait retraining phase. Subjects were asked to verbally attest to compliance with the restrictions on running activity. Subjects were required to complete all 8 sessions.
”
Because it lacked a control group, we cannotsuggest that this intervention is an improvement over hip and knee strengthening, the current standard of care for patients with PFP.
However, it is unlikely that the biomechanical changes that were noted would have occurred in the absence of the retraining. A randomized clinical trial is warranted comparing gait retraining with an intervention focused on hip and knee strengthening. Second, this study only followed the subjects up to 3 months. Consequently, the long term effects of this retraining intervention are unknown. Finally, it is unknown if the new running pattern noted post-gait retraining increases the risk of sustaining other injuries.
Our primary goal was to determine if mirror gait retraining would reduce abnormal running mechanics in females with PFP and if these changes would persist through 3 months. We also investigated if the new movement skill during running would transfer and persist in the untrained tasks of single leg squat and step descent. Finally, we sought to determine if these changes in mechanics would be reflected in improvements in pain and function. Based on these data, it appears that mirror gait retraining is an effective treatment to reduce abnormal mechanics during running. These changes generally persisted through at least 3 months. Interestingly, this new movement skill transferred to the untrained tasks of single leg squat and step descent. As with running, alterations in mechanics during these untrained tasks were either maintained or continued to improve through 3 months. Reflecting these changes in dynamic alignment, measures of pain and function improved and remained at these levels through 3 months.
Note from Rich Willy:
“What we found, but didn’t report in the paper unfortunately, was that we were cueing the runners to do something internally (squeeze their glutes) but they were thinking about doing something externally (keep the horizon from bouncing as much, pushing the walls away, etc). Essentially, the runners were finding the best, most efficient pattern for them to make the gait change. We didn’t report it because I only recorded patient strategies on the last 7 participants, so it wasn’t really a planned measure.”
Richard W. Willy, Stacey A. Meardon, André Schmidt, Nathan R. Blaylock, Scott A. Hadding & John D. Willson (2015): Changes in tibiofemoral contact forces during running in response to in-field gait retraining, Journal of Sports Sciences, December 2015
see article (Willy et al 2015 JSS.pdf):
Retrainers were asked to increase their step rate by 7.5% over preferred in response to real-time feedback provided by a wrist mounted running computer for 8routine in-field runs.
The purpose of this study was to determine (a) if a reduction in peak and cumulative tibiofemoral contact forces during running occur in response to an acute reduction in step length, (b) if a gait retraining programme using mobile bio-feedback to cue a reduction in step length results in a reduction in peak and cumulative tibiofemoral contact forces and (c) if these changes can be maintained for at least 30-days post gait retraining.
High impact running mechanics were operationally defined as running with an instantaneous load rate of vertical ground reaction forces of ≥ 85 bw · s−1 in either limb.
The impact criterion corresponds to the loading rate during running noted previously in individuals thought to be at high risk for the development of knee osteoarthritis (~5 years post-anterior cruciate ligament reconstruction) (Noehren et al.,2013)
The retraining group was then cued to increase their step rate by 7.5% while running at their preferred speed. Real-time feedback on stride rate (stride rate = step rate × 0.5) was provided via a wrist-mounted running computer (Forerunner 70™ Garmin, Olathe, KS, USA) that calculated step rate via a shoe-mounted, wireless, tri-axial accelerometer. In pilot testing, we found the step rate measurements calculated by the Forerunner 70 ™had a minimal 95% limit of agreement of−2.9 steps · min−1 and maximal 95% limit of agreement of 2.4 steps · min−1 compared with the step rate determined with our instrumented treadmill (Bland & Altman,1986). A laboratory assistant, positioned immediately in front of the treadmill, held the running computer so that the retraining participants could view their real-time step rate (Figure 1). Importantly, participants were not provided any other feedback or cueing other than feedback on step rate e.g., neither kinematic feedback nor cueing were provided. The running computer uses a 5-s roaming average to calculate step rate to provide a stable feedback value that for the runner.
Based on these data, a modest increase in step rate in response to a mobile biofeedback programme resulted in reduced peak and impulse contact forces per step for the total tibiofemoral joint and medial tibiofemoral compartment during running both acutely and after retraining. There was no change in the estimated cumulative impulse at the tibiofemoral joint or medial tibiofemoral compartment in response to the training. The results of this study provide the basis for future investigations utilising this retraining method in individuals who are at high risk for the development of knee osteoarthritis, such as those who are post-anterior cruciate ligament reconstruction or post-partial meniscectomy.
In-field gait retraining cueing a 7.5% increase in step rate during running resulted in significant reductions in tibiofemoral and medial tibiofemoral joint contact forces per stance phase, despite no changes in the knee adduction moment. Despite the increase in number of gait cycles needed to cover a given distance, there was no change in cumulative tibiofemoral joint loads. It is unknown if similar results will be found in injured populations or in those who are at-risk for the development of tibiofemoral osteoarthritis.



